Performance and Pricing of
Medicaid Non-Emergency Transportation

WHY WE DID THIS STUDY
The General Assembly directed JLARC to assess the cost-effectiveness of Medicaid non-emergency medical transportation in Virginia. Interest in this topic was prompted by concerns that poor performance could leave medically fragile Medicaid recipients vulnerable to missed appointments and reduce access to necessary health care.
ABOUT NON-EMERGENCY MEDICAL TRANSPORTATION
Non-emergency medical transportation is a federally mandated service for Medicaid enrollees who have no other means of transportation to their health care provider. The service ensures that transportation is not a barrier to receiving appropriate health care for Medicaid enrollees. Virginia contracts with a statewide broker to provide non-emergency medical transportation to the fee-for-service Medicaid population. The state spent $78 million to provide over four million trips to over 20,000 riders in FY 2015.
WHAT WE FOUND
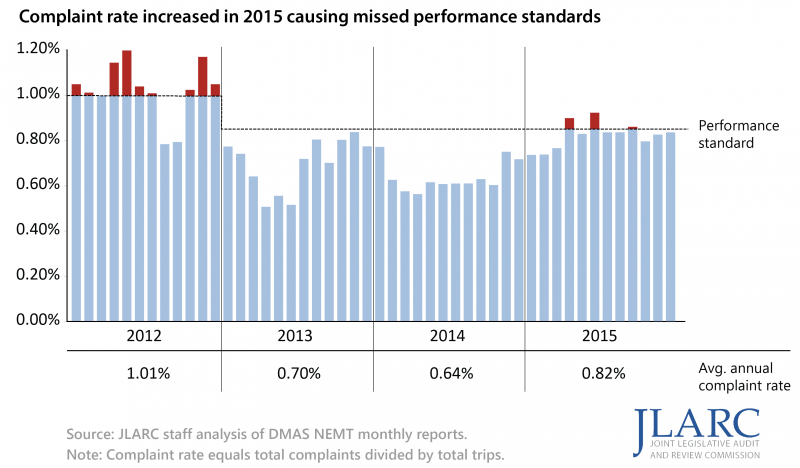
Non-emergency transportation performance improved temporarily following adoption of new standards but declined recently
The state’s non-emergency medical transportation (NEMT) performance temporarily improved after the implementation of new standards in October 2011, but subsequently declined across three critical measures since January 2014. These include a rise in complaints (most of which are due to late trips), unfulfilled trips, and late pickups upon hospital discharge. Increasing numbers of late and unfulfilled trips can put some of the most vulnerable Medicaid recipients at risk. The most common users of NEMT services are intellectually or developmentally disabled recipients.
NEMT rate setting process does not protect interests of state and Medicaid recipients by ensuring that rates reflect costs
Virginia’s NEMT rate setting process increases risk to the state, Medicaid recipients, and the broker because it does not ensure that contractually established rates reflect the cost of providing transportation services. NEMT rates were set in October 2011 for the entire contract period (up to six years), so changes in the number and cost of actual trips would have resulted in differences between actual costs incurred and the capitated rates. Overpaying for services increases costs to the state and federal governments, while underpaying puts financial pressure on the broker and providers, potentially negatively impacting performance. The state lacks reliable, independently verified data needed to establish rates that appropriately reflect costs. The current process also significantly limits the state’s leverage over negotiations if rates need to be changed, because no other short-term alternatives exist to provide required NEMT services.
WHAT WE RECOMMEND
Executive action
- DMAS should implement new contractual performance standards requiring on-time drop-off for critical care appointments.
- DMAS should require the broker to utilize a statewide GPS-enabled routing and tracking system, if it is cost-effective.
- DMAS should establish capitated rates annually using reliable, independently validated cost data.
- DMAS should have a new NEMT contract in place no later than January 1, 2016 to implement the recommended contractual and rate setting changes.
The complete list of recommendations is available here.

